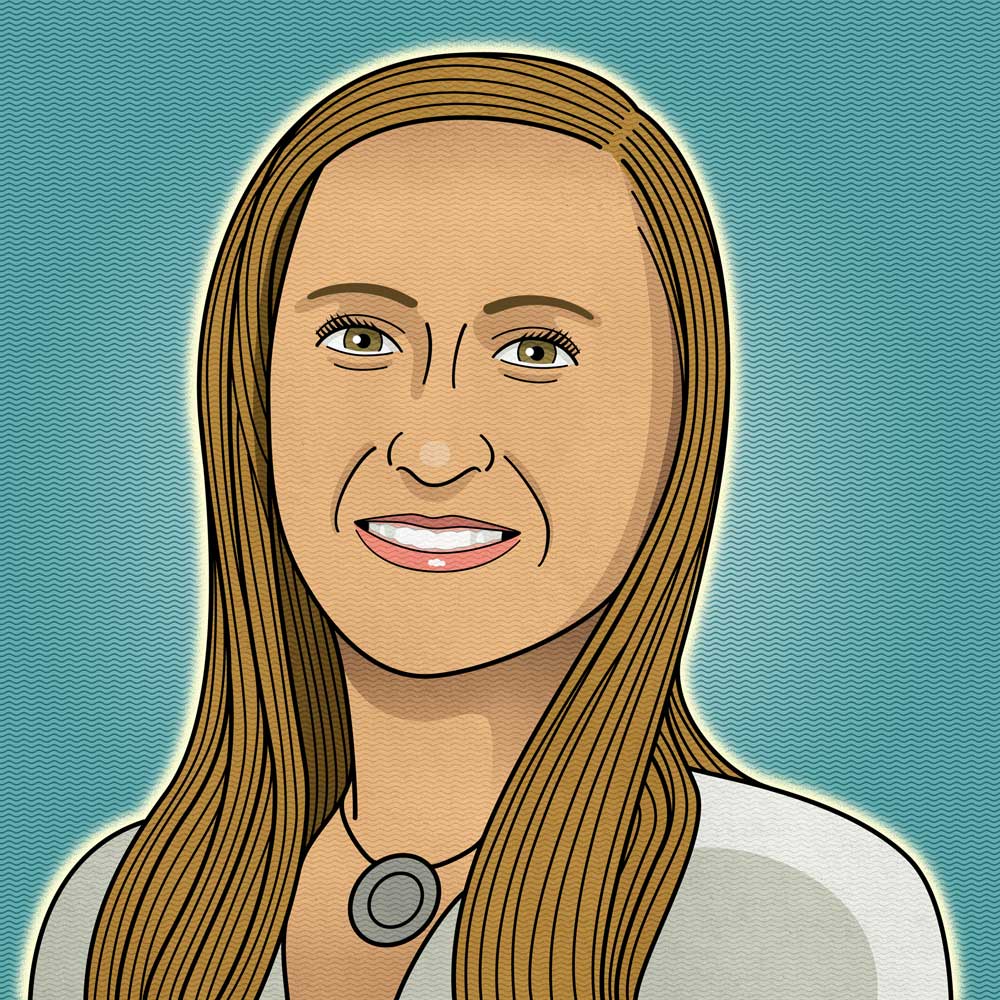
As physicians, our weapons lie beyond medications, diagnostic tools and interventions. Our weapons include our composure, our compassion and our competence. Where there is panic, we provide calm. Where there is fear, we offer courage. And where there is anger, we practice patience. We continue to stand united as a medical community despite having to stand six feet apart.
I admitted our hospital’s first COVID patient. He was alone, the blinds drawn so the city lights formed shadows across his hooded eyes, and his fear was almost palpable. I reached out a double-gloved hand and watched as a small smile began to form. “Yours is the first hand I have had the honor of shaking in this hospital and it’s cold!” he exclaimed in a hoarse voice. I laughed and responded with the old adage favored by my attending physician, “Cold hands, warm heart.” My osteopathic medical education taught me the healing power of human touch and my physiatry training coupled with my cheerleading background taught me the importance of motivation, especially in a rehabilitation setting.
With coaxing, the patient described his medical course along with his personal history. We talked about his extended Italian family, who still set a plate for him at every Friday’s pasta night, and his love for the Philadelphia Eagles. I listened intently, watching while his breathing slowed, his heart rate normalized and his smile widened. I explained the next steps in his care, from physical and occupational therapy to achieving his functional goals of gaining more independence in order to return home. The fear I sensed before soon dissipated, replaced by a new feeling: hope. He squeezed my hand, saying, “Now you have warm hands and a warm heart.”
The stress has been at times overwhelming — for patients and caregivers alike. During one 24-hour shift at the beginning of the pandemic, I had a patient who spiked a low-grade fever but otherwise had no COVID symptoms: no cough, no shortness of breath. She was on a floor where another individual had tested positive, however, so I sent for a COVID test. When it came back positive, the patient asked me if she was going to die. I reassured her that we caught the virus early and we would monitor her closely. However, it was jarring to face the realization that we were grappling with a new disease for which there simply was not enough evidence-based medicine.
The following morning, I stepped out to see chalk drawings all over the ground in front of the entrance to the hospital. There were messages that read, “’Thank you,’ ‘Heroes work here,’ ‘We appreciate you.’” I stood there with my stethoscope hanging from one hand and a paper bag with my week-old N95 mask in the other. I felt both defeated and uplifted at the same time. Reading those notes of encouragement made me cry, and I was not the only one. When you’re a doctor or a nurse, a therapist, aide or technician, this is the work you do every day. You never think of yourself as a hero or a soldier. You never think of the hospital as a battlefield. But this war is far from over and we will continue to fight to save lives. Because that is what we do, and that is who we are.
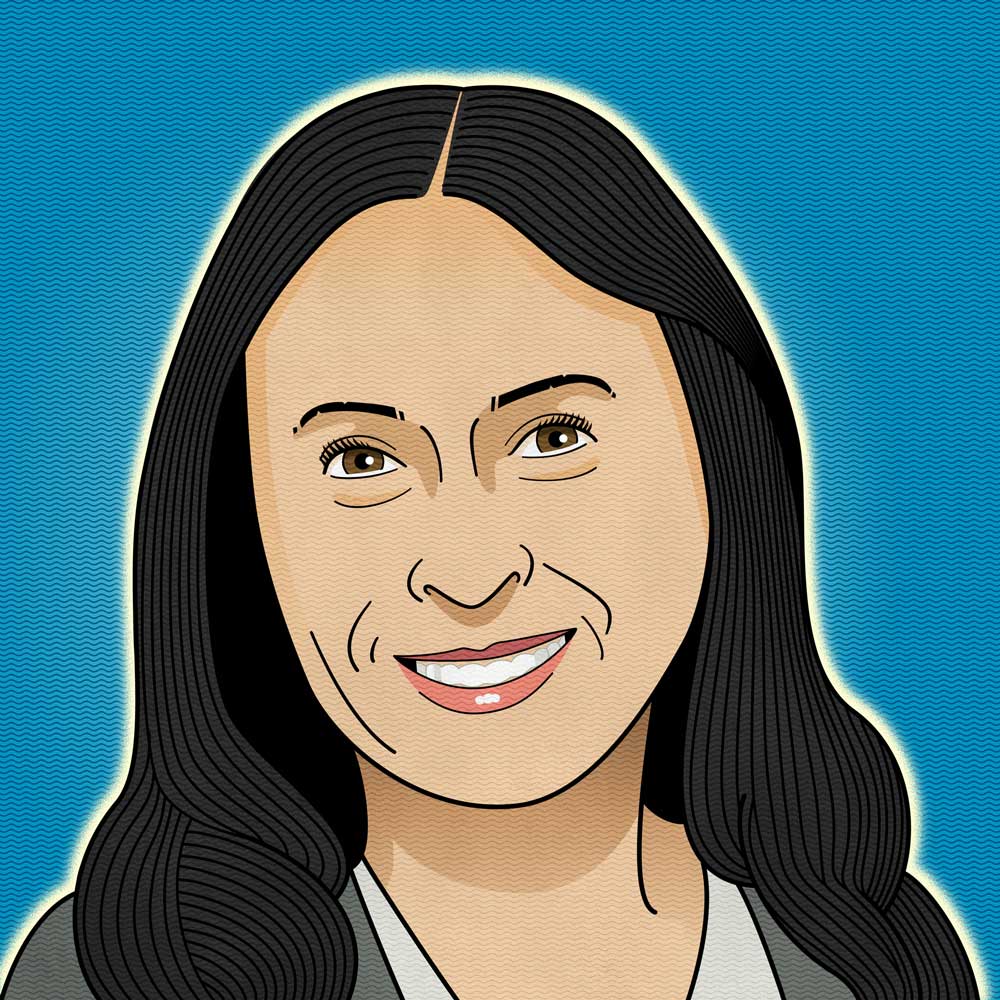
When there’s not a global pandemic, the commissioner role involves lots of policy and transformational work around strategies for addressing the needs of the state’s most vulnerable citizens. That’s important work that I hope to get to eventually, though probably not before the middle of the calendar year. But you know, among other things, what COVID has done is to really put the spotlight on gaps that have existed in our system and the people who fall into those gaps, such as individuals in our homeless population. A COVID diagnosis for them is particularly complicated, especially in winter.
My days right now are filled with crafting the plans that allow people to get tested; making plans for surges in hospitals and standing up alternate care sites; figuring out how to provide vaccines to more than a million people; and problem-solving critical staffing issues at nursing homes. Each commissioner is different, depending on her or his background, but mine happens to be in operations, and as a nurse. So I feel very comfortable getting right into developing and executing operational plans. My passion is caring for vulnerable people, and when my term is over, I’ll return to some sort of caregiving role on the other side of the commissioner’s desk. For now, this particular role allows me to care for more of them.
We’ve covered a lot of ground since the start of the pandemic and have a much better understanding now of so many things: how to test, how to isolate and quarantine, how our hospitals can manage a surge in cases internally, how to stand up alternative care sites in as little as 24 hours. What keeps me up at this point is our long-term care facilities and the challenges their residents are facing. Illness, isolation, lack of engagement, loss of life. We hear a lot, of course, about those who succumb to COVID, but as tragic to me is the fact that we have so many long-term care residents who — even though they aren’t ill — haven’t been able to be with their families in any meaningful way in almost a year now.
The hope I’m holding onto is that we’ll come out on the other side of the vaccine with a renewed energy to live our best life. I know I’m certainly looking forward to when my life goes back to normal.

Even when the virus spread to Europe and the United States, I was still thinking it would be fine: the CDC would do what it always did and oversee the national response while providing local and regional public health departments with guidance and support. I said as much in an interview in February. Having worked with the CDC inside the Global Disease Detection Unit during the 2009 H1N1 pandemic, my assumption was that they were prepared with a strong and effective coordinated response.
And then I got sick. I woke up on March 1 with a sore throat and fatigue, and four days later, I was running a fever of 102.5. I ended up in the ER on March 9 with a fever, dry cough and tightness in my chest. After negative flu and strep tests and a chest x-ray that looked clear, I was sent home to quarantine, and when I didn’t get better, I returned to urgent care on March 15. That was the oh-no moment for me: the doctor on call said she’d have tested me for COVID if she could, but she had zero test kits available. When I called my regular doctor, she said my risk profile was too low to justify using one of the very limited kits she had to test me.
The realization that there was virtually no testing available made it clear to me that our country was botching the pandemic response. The most important thing is testing; you can’t respond to what you can’t see. In April, I went on CNN to talk with Anderson Cooper about the pandemic, publicly walking back my February assertion that the United States was in a position to handle it. The chyron that ran under my image read: “I COULDN’T HAVE BEEN MORE WRONG.”
Ultimately, it turned out that I didn’t have COVID; over the summer, when testing became more broadly available, I had a negative antibody test — and a positive titer for Epstein-Barr, or mono. As of late January, however, we’ve lost more than 400,000 Americans to COVID — fully 20 percent of the 2 million global deaths attributed to the pandemic — and if I have one message, it’s this: there’s nothing more important we can do to protect ourselves from future pandemics than funding public health. If public health is doing its job, it’s the first thing to be cut — because, well, nothing is happening. But if the past year has demonstrated anything, it’s that we should be funding public health programs the way we fund national defense programs, because public health is national defense — against deadly pathogens like SARS CoV-2.
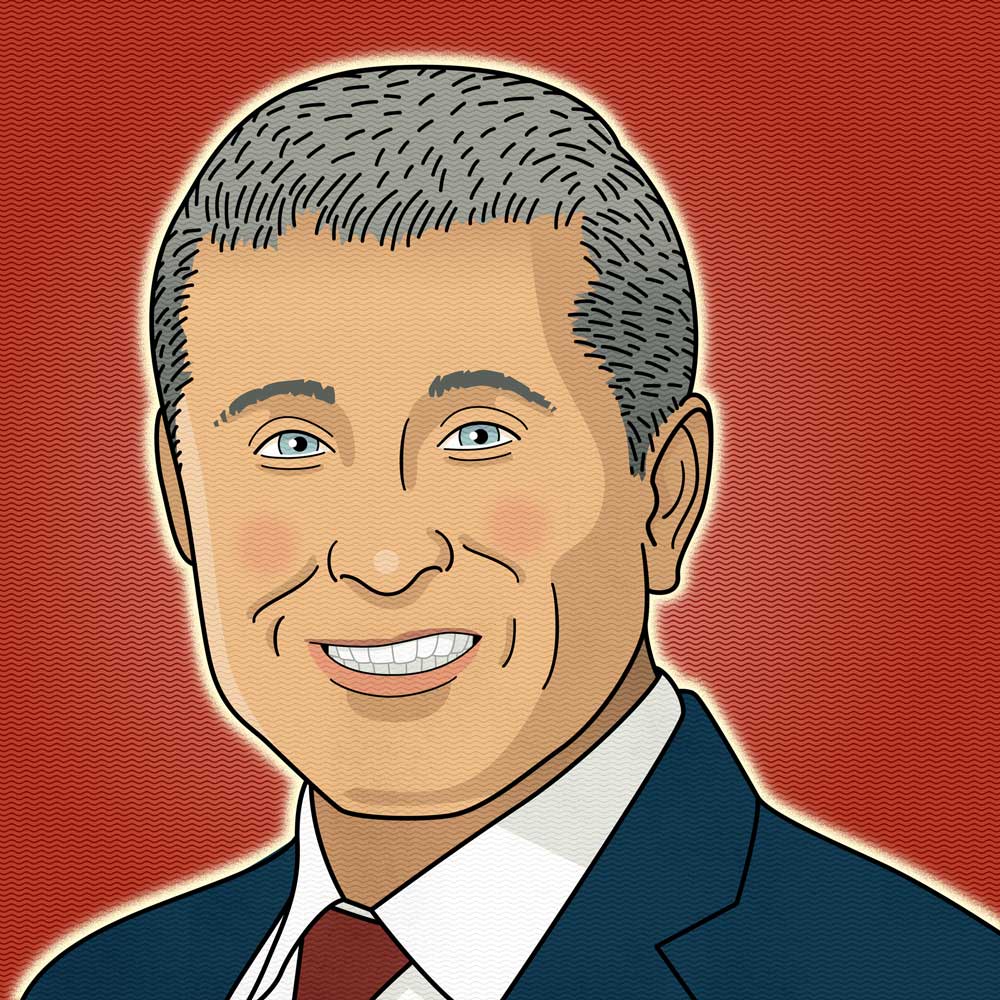
I was in the MGH medical ICU for 32 days, though I have exactly two memories of that time. One was hearing my daughter Hadley’s voice during a FaceTime call. The other is a nurse coming up to me as I left the hospital for Spaulding Rehab to give me a hug and saying something like, “I’m probably not supposed to do this, but I can’t not hug you.” She’d obviously taken care of me at some point during my hospitalization — maybe a lot of it — but I had no recollection of that. At the Spaulding, a calendar on the wall said it was late April and I was shocked. The last thing I knew, it had been March 13.
Honestly, I really didn’t get a full understanding of my story — how sick I’d been, how close I’d come to dying — until the New York Times wrote about me in May. I’d been on ECMO [extracorporeal membrane oxygenation; a last-effort lifesaving measure used to pump oxygen into patients’ blood when their own lungs aren’t capable of doing so] and every medication that was available at the time. My lungs were completely whited out — one of the worst chest x-rays one of my doctors had ever seen. Even turning my body to prevent bedsores was enough to make my oxygen level crater. At one point, Kim asked the medical team for an honest assessment of whether I’d survive and they told her it wasn’t likely. She told me later, though, that she always knew I would come home. I give her so much credit — she was just a rock for our family, strong, focused and positive-thinking.
The people who have been on the COVID frontlines are heroes. That’s a term that gets thrown around lightly, but I really mean that. I’ve always had an appreciation for the medical community because of the work I do, but after the past year — not just knowing about my own experience, but hearing about the way people are putting themselves out there day in and day out, putting their own health and safety at risk … it’s even more personal to me.
Today, I’m doing fantastic. I’m completely recovered. I’ve always been an active, outdoorsy person — biking, running, hiking, skiing — and I’m back to all of that. I even caught my first tuna last summer, so 2020 wasn’t all bad. I live my life, but I do it safely.
During those initial weeks, everybody was anxious, on edge. All the flags were up. It was particularly challenging knowing we couldn’t rely on the tests, even as we had to be judicious about our use of PPE. Now, we know so much more about what to do and what to expect, but there are some challenges inherent to caring for COVID patients that haven’t changed. As a provider, preparing yourself to go into that patient room, you have to be meticulous and make sure you’re protected — but you also have to keep foremost in your mind that this is a person, and one who’s not only extremely ill, but also isolated and likely very scared. You feel like an alien, and your patient feels alienated. COVID has really challenged our ability to express compassion and connection through the human touch, and that’s a huge loss. It’s important for us to hold on to our humanity in spite of the physical barriers that come between us and our patients.
And then there are our other patients, the ones who have non-COVID needs. When the pandemic erupted, the whole world kind of stopped, including most primary care practices. As an infectious disease practice, ours was one of the only offices that was able to stay open. While telehealth visits work for some needs, there were many patients whose care was put on hold; whose care has suffered, like the diabetic patient whose A1C hasn’t been measured for months and has been working on a foot ulcer that’s now septic. Chances are you’re not going to see — or smell — that toe during a telehealth appointment, just like you’re not going to pick up on another patient’s heart murmur, or any of a hundred other things you only catch in a face-to-face visit. It’s felt overwhelming at times, stepping out of my specialist role to serve essentially as some patients’ primary care provider, but it’s what the situation has required.
The past year has been grueling, to say the least. Of the four providers in our practice, we have only two full-time equivalents seeing patients, and we’re covering a multiple of our typical patient load spread across the hospital and several outpatient locations. Work has been pretty much my be-all and end-all. Fortunately for me, relaxing is not in my vocabulary.
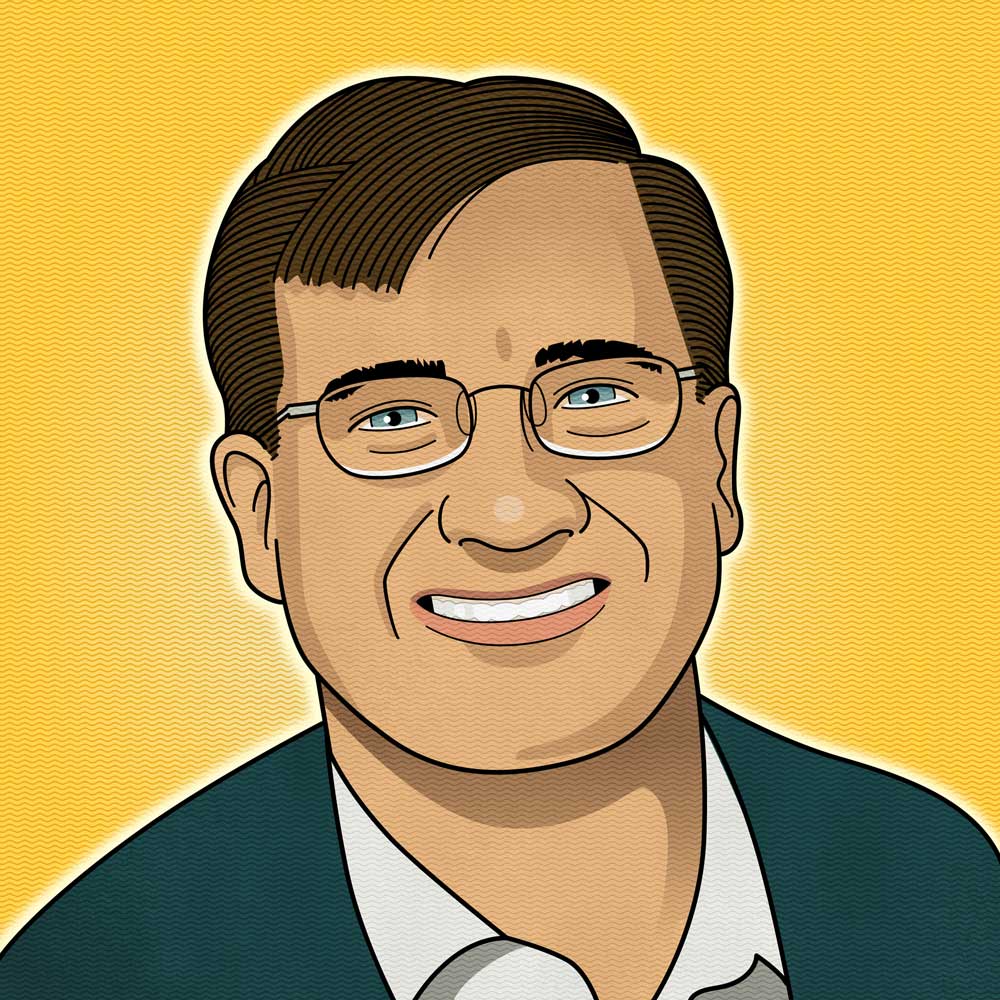
Standing up our own lab was challenging but not complex. We needed it to do one thing — run a reverse transcription polymerase chain reaction test, the so-called “gold standard” molecular diagnostic test for COVID-19 — and we needed it to do it thousands of times every day. I knew how to build a lab; before I came to UNH, I ran a biotech company in North Carolina and was well-versed in the business of science and the science of business. Honestly, the biggest challenges were logistical: understanding the supply chain, figuring out how to identify and track and report results on 4,000 tests per day (the answer, if you’re wondering, is barcodes), knowing what equipment and materials to order before we actually needed them. There were other schools that wanted to stand up their own labs, but by the time they decided to act, it was too late: they couldn’t get the equipment in time, or even at all. It wasn’t that we got lucky. It was that we had the right people with the right skillset in the right place at the right time. It was almost like it was meant to be. There was a team of 50-70 people across UNH who basically stopped doing their day jobs to make sure we got this done. It was UNH at its finest.
UNH has the best testing program in the world. I really mean that. Testing in the volume we do — every student, twice a week — last fall allowed us to identify asymptomatic cases before they led to outbreaks and to maintain uninterrupted operations through the end of the semester. There was literally only one day the entire fall when the infection rate on campus exceeded 1%. We didn’t do everything right, of course, and we took the semester break to refine some processes that will allow us to be even better, but still — an infection rate below 1% is pretty much unheard of. Our students did what we asked of them, Kelly Thomas [the lab’s director and UNH’s Hubbard Professor of Genomics] was dead-on right with every call he made, whether it was about pooled testing or PCR —. People ask and I tell them our campus is the safest place to be in the entire state.
We don’t have a med school. We don’t have a vet school. We don’t have a pharmacy school. We actually did not have a reason to think we should be able to do this except we’re in New Hampshire, and we just do stuff because we know that it needs to be done. And my biochemistry degree from UNH sure didn’t hurt!

Feb. 1, 2020, was the day we activated our public health incident response team, following information coming out of the Centers for Disease Control and the World Health Organization that COVID had reached the United States and was spreading rapidly. That meant both preparing for an outbreak — readying surveillance systems, assessing laboratory capacity, developing public communications, training staff, getting a handle on what and where our most vulnerable populations were, and more — as well as laying the groundwork for handling the outbreak itself: investigating cases, doing contact tracing, developing containment measures and contingency plans for hospitals that might reach capacity during a surge, creating a roadmap for vaccinating the public.
Through last June, I was working every day, long hours, to help stand up and maintain our contact tracing program. After that, we had a reprieve for a stretch through the summer while our case counts were low, but the work started to pick back up again in the fall as community COVID-19 transmission increased and vaccine planning activities ramped up. While some of us are the public “face” of the response, there are so many people across this entire response team who have been putting in incredible hours to do the work that’s necessary to respond to this pandemic. Not to mention all of our healthcare heroes on the front lines of caring for patients with COVID-19.
Fortunately, my family has been incredibly understanding. My husband is also an essential worker— he’s a police officer and has had to work a difficult schedule too. We have made it work. Obviously, I haven’t been able to be home as much as I would like this past year, but my kids understand that what I’m doing is important. I hope they’ll remember this period as a time when our family made sacrifices in support of public service.
We’ve been preparing for a pandemic in New Hampshire for more than two decades, but I didn’t think we would find ourselves facing such an extended public health response. And of course, there’s a big difference between planning for a pandemic and actually responding to one — you learn things along the way that change your approach. One of the biggest things we hadn’t fully planned for was the amount of testing that would be needed. As of Feb. 1, we’ve conducted 1.3 million tests for COVID-19 in the state, testing more than 600,000 people. That’s not something we had a plan for; there’s never been an outbreak that required testing on this level. We had alternate care site plans, we had vaccine rollout plans … but there wasn’t some massive-scale testing plan we had sitting on a shelf somewhere that we could dust off and put in place for this. It’s been remarkable to see all of our partners come together and help implement these plans and our response. These partnerships have been essential.
I worry a lot about the human impact — the lives that have been lost, the prolonged isolation, the financial hardships that so many of the state’s residents are facing. At the same time, I really appreciate the way people have responded to the challenges … it’s given me a lot of hope. By and large, people are taking this incredibly seriously: following the rules, wearing masks and social distancing, staying home if they have been exposed or when they think they might be ill. And now we’re vaccinating. Over the next few months, we’ll have our most vulnerable citizens vaccinated and will get everyone else who wants to be vaccinated in time. I feel hopeful about that, too. We are going to get through this.

Generally, people think of the immune response as a positive, and generally it is. In the broadest terms, it’s the body’s recognition of substances that appear foreign and harmful — in the case of COVID, viral proteins. These proteins are then targeted by antibodies: glycoproteins (sugar proteins) that recognize these foreign substances and neutralize them, and then continue to circulate in the blood, providing protection from future exposure. There are instances, however, in which the immune system over-responds to these foreign invaders, producing antibodies that actually exacerbate, rather than mitigate, viral diseases. Two such processes are called “antibody-dependent enhancement of infection” and “cytokine storms.” The question we are looking to answer is whether these phenomena might be occurring in patients infected with SARS-CoV-2 because of specific antibody receptors, thus providing at least one explanation for why some people with COVID-19 get so much sicker than others.
One thing that’s important to understand is that the antibodies that humans make in response to viral infections come in lots of different “flavors,” if you will, and they vary a bit from one person to another because genetically we’re all a little bit different. One of the “flavor” differences is the type of sugar molecule that’s attached to these antibodies, and recent studies indicate that antibodies lacking the sugar fucose seem to be causing the most trouble: specifically, they trigger cytokine storming which is an excessive inflammatory reaction that causes lung injury, multi-organ failure and other unfavorable outcomes in certain COVID patients. And it turns out they’re doing that by interacting with the exact antibody receptors that we were looking at.
Right now, our study is small — from an initial pool of 40 donors, we ended up with only seven people who fit our criteria. The next step is to expand the data set so we can publish our results, and then hopefully determine mechanisms that can prevent the severe cytokine stormers from making so many cytokines. Medarex, the company I started, spun off a biotech that’s now the biggest antibody manufacturer in the world. Among other things, that means if we get data that supports the idea that specific therapeutic antibodies could prevent cytokine storms in COVID, we could get those antibodies made in a month.